|
By Duke Autret, Myotherapist
It’s important to recognise and understand that musculoskeletal health and pain is highly influenced by the overall health, function and condition of the body and its context or environment it lives within. The Biopsychosocial (BPS) Model is a holistic and interdisciplinary approach to understanding health and illness that considers the biological, psychological, and social factors that influence our well-being. One key component of the BPS Model is the concept of "predisposing and perpetuating factors" that can lead to the development of conditions or worsen existing ones, making it harder to recover. In this article, we will explore the most common perpetuating factors and their relation to the BPS Model. These determinant factors of pain can be classified into different categories such as metabolic, social, and physical factors. Let's take a closer look at these factors: Metabolic Factors Hormonal imbalances, poor nutrition, and chronic diseases can contribute to the onset and perpetuation of pain.
Psychological Factors The breadth of psychological, cognitive and emotional health factors are beyond the scope of this article however here are some examples as food for thought.
Social Factors Our social connections and relationships play a most significant role in our overall health and well-being. A lack of social support or unhealthy relationships can contribute to the perpetuation of pain. Our social connections and the quality of our relationships have a significant impact on our mental and physical health. A lack of social support or unhealthy relationships have also been linked to a range of health problems, including depression, anxiety, forms of dementia, and heart disease. The social factors of health cannot be underestimated, in fact a whole host of studies have linked social isolation to being the biggest health risk today, especially for middle-aged men! In the BPS Model we recognise the importance of strengthening social support networks as part of a comprehensive treatment plan. Physical Factors Physical factors such as inactivity/sedentism, load, and motor control can contribute to the perpetuation of pain. The BPS Model acknowledges the importance of addressing these factors by exploring ways to increase physical activity levels, optimising load levels, and assessing and addressing motor control issues through refining movement patterns, alignment, and body awareness.
By understanding the perpetuating factors of pain and their relation to the BPS Model, you can take steps to improve your overall health and well-being. Remember, pain is not just a physical symptom but can also be influenced by psychological and social factors. By addressing all aspects of your well-being, you can achieve long-term pain relief and optimal health. If you are experiencing pain, it is essential to seek help from healthcare practitioners who take a holistic approach to your well-being. By considering the biological, psychological, and social factors that contribute to your pain, a comprehensive treatment plan can be developed that addresses the perpetuating factors and promotes your overall health and well-being. Our friendly staff here at Simple Wellness are all trained and well versed in this approach and are here to help you with your health needs. By Peter Pascalis We know that pain sucks, right? We also know that if our body/mind didn’t produce pain we would probably not be too well or even able to read this blog right now. You see pain serves us by alerting us that there’s something wrong which requires our attention. So, we understand that pain is an important function for our survival and for health but when does pain become a pain in the proverbial? Well, most people who suffer from chronic pain would understand the reality of having to experience discomfort daily. For others it might come and go, but regardless of its presentation something interesting happens in the body when pain evolves from purely alerting us of harm, to becoming the harm that we perceive to be threatening our survival.
We call this chronic pain but also pain which is mediated from our brains. That’s not to say that pain exists only in our brains because obviously when some part of our system is injured there’s a legit reason for having it. The processing of pain occurs in higher brain centres where our values, beliefs, understandings, expectations and experiences exist. This is where we give value to the threat: when will I be able to swim or run again, and what will this mean to my fitness goals? “Oh God I’m going to put on so much weight”. This leads us to catastrophize, and this adds further negative input into an already sensitised nervous system. Fortunately, there are solutions to reducing the likelihood of acute pain progression and that’s where physical therapy can help. Using various treatments, manual therapy can change the way our brain perceives threat by decreasing the sensory stimulus it receives. The mechanism by which this is done is by the stimulation of fast acting sensory nerve fibres which intercept the pain signals from the slower conducting pain sensing nerve fibres. By modulating pain signals, we lower the volume on those painful stimuli which can reduce the level of pain experienced. The mechanisms by which manual therapy creates changes to the neurophysiological system are:
This provides us with a window to which we can address altered muscle and postural imbalances aiming to resolve what led to the pain appearing in the first place. Myotherapy is a holistic manual therapy approach for the treatment of painful musculoskeletal conditions which considers the mechanism of pain and provides tailored solutions for its treatment and its resolution. As therapists we use the above concepts to help change your pain experience through hands on therapies, tools like cupping and needling, exercises and modifications to your daily activities. If you are experiencing pain and are looking for a solution out of it now, we are here to help. Book your consultation and treatment with any of our therapists and we will guide you through a treatment plan customised for you and your specific circumstances. Whether you’re an athlete or a weekend warrior, an injury can set you back when it comes to your exercise goals. How you handle an injury can make a big impact on the recovery process. If you want to speed up your recovery and minimise the risk of injury in the future, this is the guide for you.
What to do immediately after an injury So you’re reading this right as you’ve hurt yourself. Props to you for Googling the answer! But on a serious note, it’s good to have the injury assessed by a GP if you suspect a fracture, dislocation or muscle tear. That way, you know right away whether you will need any significant treatment such as surgery or a cast. In the meantime, start with elevating the injured body part. This helps to reduce fluid retention in the area. It also means you’re not on it, so you’re less likely to keep injuring it! Rest and elevation are also a good idea for minor injuries such as sprains and twisted ankles. If you have a pre-made support or brace for the injured part, you can pop it on for some stability and compression. If not, you might like to bandage it if compression feels supportive for you. There is a bit of debate out there about whether heat or ice is best for an injury. Ice is the old-school treatment, and may be useful for reducing pain sensitivity and fluid retention. On the other hand, if there is pain without any swelling, a heat pack or warm bath might help increase blood flow to the area and reduce pain. Once the swelling has gone down This is the time when it’s good to see your friendly local myotherapist. We can’t really help if you’ve just done a significant injury such as a break or a muscle tear. But after the first few days, we can put together a treatment plan to get you back to your everyday life ASAP. Some of the therapies we can offer to help you recover include:
How to support recovery and reduce risk of re-injury Are you ready to jump back into it after an injury? Here are some tips to maximise recovery and minimise your risk of getting hurt again. Start slow – I know you want to jump straight back in, but this is a recipe for disaster! When you’ve been injured, your body part often needs time to strengthen and get back to your pre-injury levels. Begin with low impact versions of movement such as yoga and walking, and build up over a period of 4-12 weeks depending on your injury. Use rest and compression after exercise – if you do find your injured area aching or swelling after exercise, head home to rest and a support or brace. This can minimise the fluid retention and ease any pain you might experience. If you experience sharp or shooting pain, stop – some aches are common as you get back into movement. But sharp, shooting or severe pain is a sign that something is not ok. Stop whatever you’re doing until your pain has been checked out by a qualified practitioner. Eat plenty of nutrient-dense foods – even if your rehab program is perfect, your body can’t recover without the good nutrients you need for healing. Eating plenty of fruit, veggies, nuts, seeds, herbs, spices and high-quality is protein is a good start, according to our nutritionist friend Samantha Gemmell. Work with a myotherapist – a myotherapist can help you with rehab exercises to rebuild strength. But they can also keep you on track with supportive taping and addressing any muscle imbalances. Are you dealing with an injury? Our myotherapist Emily works with people with sports injuries, particularly muscle tears, joint injuries and rehab. Her goal is to get you back to training, events and everyday life as soon as possible while minimising your risk of re-injury. To book an appointment with Emily, head to our booking page and select ‘Emily Wells’ as your practitioner. Nobody likes to feel sore and achey all the time. If you experience chronic pain, it can contribute to many other conditions and sabotage your mental health. But if you’re looking for natural ways to relieve pain, the first place to look to is your diet. My good friend and incredible Nutritionist, Sam Gemmell, has taken the time to write this guest blog to explain more. Oily fish
Fatty fish are a potent source of omega-3 fatty acids, which are naturally anti-inflammatory. Most studies that have been published focus on omega-3 supplements. But there are small studies that support consuming it as part of the diet as well. One showed that consuming fatty fish 4 times per week can reduce inflammatory compounds in the body. 3-4 serves of oily fish per week is a good number to aim for. If you prefer plant-based sources, include walnuts, chia seeds, flaxseeds and hemp seeds daily to reap the benefits. Olive oil Looking for a healthy source of fat to include in your diet? High quality olive oil has properties that may help to reduce joint-related symptoms. One animal study showed that extra-virgin olive oil reduced joint swelling, slowed the destruction of cartilage and reduced inflammation. But don’t worry – the benefits are for people as well! One study showed that people who consume olive oil are less likely to have rheumatoid arthritis. Olive oil can be drizzled over salads, or used to sauté ingredients. But it's not great for deep frying - deep frying isn't good for you anyway! Berries Berries are the best fruit ever, at least in my opinion! They are chock-full of nutrients including vitamins, minerals and antioxidants that can help to reduce inflammation naturally. One study showed that people who ate at least two servings of strawberries per week were 14% less likely to have elevated inflammatory markers. Researchers also suggest that blueberries and strawberries may offer protection against arthritis. Want to up your berry intake? Chuck them in your smoothies, porridge, salads or just straight into your mouth. Spices Spice things up in the kitchen! Pretty much any herb or spice will have antioxidant and anti-inflammatory properties. But if we’re going to play favourites, turmeric and ginger are bestfor sore joints and arthritis. There are many research studies that show supplementing with turmeric can be beneficial for arthritis. But adding it into your diet can still help as well! Turmeric is not well absorbed, so the best consume it is with a source of good fats and some black pepper. Research into turmeric and ginger has shown that both have anti-arthritic effects. How to use them? It’s simple – sprinkle your favourites spices everywhere! Turmeric and ginger can be added to sweet and savoury dishes. Tart cherry juice Tart cherries are packed full of antioxidants that can support your joint health. One study looking at osteoarthritis showed that consuming 475ml of tart cherry juice daily significantly reduced symptoms and inflammation. Tart cherry juice can also reduce inflammatory markers. But the benefits don't stop there. Tart cherry juice is also a natural source of melatonin, which is needed for deep, restful sleep. If you’re not getting quality sleep, your body can’t repair damage effectively, which can exacerbate pain. Ready to get into tart cherry juice? Make sure you choose an unsweetened variety. Otherwise, a lot of the benefits will be cancelled out by excess sugar. Green tea Don’t get me wrong, I love my coffee. But green tea is king when it comes to caffeine-containing beverages if you’re in pain. Green tea contains a potent antioxidant known as ECGC. ECGC has been shown to reduce inflammatory cytokines in research. And although trials are in the early stages, the research also suggests that it could be beneficial in reducing inflammation in osteoarthritis. I often recommend that coffee drinkers alternate between coffee and green tea – so if you drink 4 cups of coffee per day, try 2 cups of coffee and 2 cups of green tea. But if you're not big on caffeine, even one cup a day can offer health benefits. About Sam Sam is a nutritionist, health writer and wellness speaker based in Melbourne. She loves to spread knowledge about food as medicine, and is passionate about personalised nutrition. You can find out more on her website. There are many different issues that can cause pain around the jaw and face. In fact, between 5-12% of people experience some kind of dysfunction in the temporomandibular joint (TMJ). But the good news is, TMJ pain doesn’t have to stick around. What causes jaw pain?
There are many factors that can contribute to pain in the jaw and around the TMJ joint. This can include:
Your jaw pain could be caused by one or more factors, depending on your situation. Symptoms of jaw pain If you have dysfunction in the TMJ, pain is an obvious symptom. But there are other symptoms caused by jaw issues to keep an eye out for, including:
You could also experience symptoms that come with generalised pain, such as nausea, lack of appetite, irritability and fatigue. Assessing jaw pain If you’re experiencing jaw pain, your best bet is to see your friendly local myotherapist (that’s me!). There are a number of things I will do to assess the pain. We’ll look at:
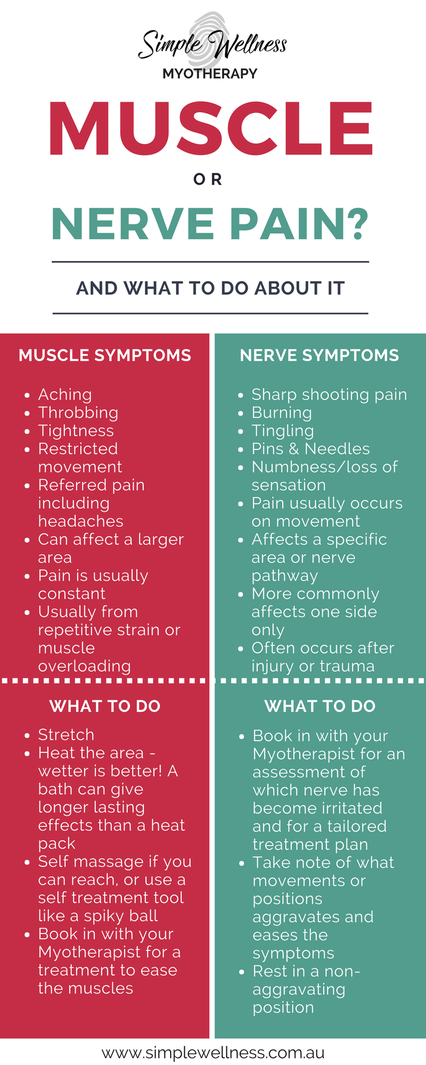
There will also be some palpation, or feeling, of the jaw. This will tell me whether one side is tighter compared to the other, which may be maintaining your jaws dysfunctional patterns. What can be done to ease jaw pain To get to the bottom of the TMJ issues, you’ll need to see a practitioner for assessment and treatment. But if you need some immediate release for your jaw pain, you can try this self-release technique. Start with your fingertips pointing upwards on the base of the jaw. Press your fingertips down firmly (but not painfully!). You might feel a hard sensation - that is the tightened muscle. In one long, slow movement, roll your fingertips up the jawline, over the cheek and cheekbones, along the temples and up to the hairline. Do this slowly and deeply, taking 1-2 minutes from jaw to hairline. Open and close your jaw wide like you’re yawning. Then repeat the process 1-2 times. In myotherapy, treatment of jaw pain may include mobilisation, myofascial release, trigger point work and intra-oral release. Intra-oral release is an internal treatment – I’ll get gloved up, and then use my finger or thumb to release the tight muscles of the jaw from inside the mouth. This can be painful – I’ve had it done to me as well! - but it is effective for the majority of clients with TMJ pain. In my own TMJ treatment experience, I was having extreme tightness and pressure build up in the joints of my jaw. When I opened my mouth my jaw swung noticeably towards the left. When it got bad, it was a struggle to eat things like nut bars or anything that requires a lot of chewing. It took time, but between seeing my own Myotherapist and doing the self care exercises he gave me, I've mostly corrected the dysfunction and its very rarely painful anymore. If you’re ready to release your TMJ tension, book yourself in for a session today. Pain is sucky – no matter what it is. But sometimes it’s good to know your pain, so you know how urgently you need to act on it. One of the most common questions about pain is how can you tell if it’s muscle pain or nerve pain? The best option is always to ask someone who can check for you – like me! But there are some ways you might be able to tell the difference. Muscle Pain It’s pretty common to experience muscle pain. It might be as subtle as an ache after a workout, or it could be agony if you’ve torn a muscle. The way to recognise muscle pain is that it is generally:
Nerve Pain Nerve pain is usually of greater concern, as your nerves hurting is a sign that something is compressing or impinging a nerve somewhere in the body. If you’re experiencing nerve pain, it is generally:
The two types of pain can exist separately, or you might experience a mix of both. But both are a sign that the body is not happy with something. I’m In Pain Right Now. What Can I Do To Relieve It? Pain is a signal that lets you know something might not be right and needs protection. If it’s a mild pain, there’s no need to panic. But if it’s unexpected pain, nerve pain or related to a chronic condition, your first step is to book in with your practitioner. Getting treatment right away helps to reduce your pain quicker. Your practitioner can advise you on some safe at home care practices, but if you can't get a booking at short notice there are still steps you can take. Whether its muscle or nerve pain, the basic DIY first aid for your pain is the same. So until you are able to get it looked after, you should:
These will help to ease the pain and prevent further damage until you’re able to get in and get it checked out properly. You’ll see that I didn’t include ice in there. There is emerging research that shows that ice may not always be the best option for treating injuries and pain. So if you want to add on some temperature relief, it’s up to you – you might feel like ice gives you some relief, or you might prefer a heat pack, or you may find best relief using an alternating combination of the two. Once I’ve assessed your pain, I will let you know which might be better for you. The guide below is a quick way of doing the investigative work on whether your pain is muscle or nerve related, but its always best to consult with a health professional rather than trusting good old Doctor Google. You don’t have to just grit your teeth through any sort of pain. As a qualified myotherapist, I can help to relieve your symptoms and get you back on track to health. So book in an appointment today – you won’t regret it!
Is myotherapy painful if it's done 'right'? Should massage hurt in order to be effective? These are the sorts of things I get asked all the time. As a practitioner with a strong interest in the world of chronic pain, I get very passionate about this topic. So apologies for the rant ahead! The myth
Somewhere along the line, people started to equate pain and gain. It's in the workplace, in the gym, and now even on the treatment table. There are many who think a 'good' massage or myotherapy treatment should make them wince. They think that:
But is this really the case? The reality Does pain really equal gain? I don't think so – particularly not for people already in pain. If you're already experiencing pain, your nervous system is already on overload. And that means you're already vulnerable to more pain. Pain is not a healthy thing in large amounts! In fact, when your body experiences pain, you'll have:
I don't know about you. But I think that if you walk out of a chronic pain treatment with more inflammation, fewer nutrients and more stress – it might not be a good choice for your healing. On the other hand, a gentle treatment that lowers stress hormones and inflammation might be just what you need. Can you have a pain-free treatment? I believe that you can have a low-pain, if not completely pain-free myotherapy treatment. There's a few ways you can make sure that this happens:
You might still experience some sensations like tenderness on trigger points, or mild discomfort during a stretch. But that's not quite the same as pain – I'll explain in a later post. Are you still worried about pain during a treatment? I want to hear your concerns and let you know how I can help. Send me a message, and we can talk about how to keep you pain-free. Ready to get yourself a gentle AND effective treatment for your pain? Pop on over to the booking page to get started. |
Meet Our Team
We have a team of great practitioners available 7 days a week at our Rowville clinic. Archives
July 2024
Categories
All
|
Got a question about Myotherapy?
Contact Mel by phone, email or Facebook
|
Simple Wellness Myotherapy & Remedial Massage Clinic
Shop 12B 150 Kelletts Rd Rowville VIC 3178 |
Phone us on
03 8204 0970 |





 RSS Feed
RSS Feed