|
Many people are familiar with the term "bulging disc" in regards to lower back pain. It can feel like an intense, sharp, stabbing sensation that can often travel down your leg through your hips and bum, sometimes as far as your feet. This is a common diagnosis when you start to develop back pain. You get a scan which shows changes in the disc, and the pain matches the effected nerve area. It can be a scary diagnosis. But you may be surprised to know that a lot of people who don't have pain have also been found to have changes in their discs. I find this study to be really encouraging, because it shows that people who have significant changes to their disc structure can still live a painfree life. It suggests that the disc changes may have already been there for some time before any painful symptoms even began, and gives hope that even if the structure doesn't change, that the pain can change. Lets have a look at this interesting literature review, particularly in regards to the findings around disc degeneration, disc bulges and disc protrusions. This is a literature review of 33 separate studies that investigated the imaging of spinal degeneration in painfree people ranging from their 20's to their 80's. It was published in the American Journal of Neuroradiology in 2014. In total, the review takes into account MRI and CT scan imaging on 3110 individuals with no painful symptoms. As you would likely predict, the number of findings increased with the participants age group, showing age-related degeneration occurs even in people who aren't experiencing pain. Lets have a look at the imaging results for the disc degeneration, bulge and protrusion categories: Disc degeneration - changes to the disc and surrounding vertebrae that result in loss of cushioning and support, may include signs of osteoarthritis at the joint. The Results: Disc degeneration in painfree participants was identified in:
Disc bulge - changes that alter the shape of the disc and can make portions of it "bulge" out of place, which can apply pressure to nearby nerves. The Results: Disc bulge in painfree participants was identified in:
Disc protrusion - changes to the annular membranes around the disc allows the disc nucleus to protrude and apply pressure to the nerves. The Results: Disc protrusion in painfree participants was identified in:
What does this mean for your bulging disc? It means that theres a good chance that your structural changes were already present before your back became painful. The area may be irritated or flared up right now, but these findings are a good indication that even if your scans don't change, your back pain still can settle down. It means that a scan showing disc changes doesn't have to be a life sentence of pain. Does this mean bulging discs DON'T cause pain, then? Don't get me wrong, bulging discs can be painful, and for some people it can be severe. This study just helps to show us that theres more to back pain that what shows up on MRI or CT scans. Structural changes are just one layer in the complex onion that is back pain. We can help! There are lots of ways we can change your experience of back pain through massage and myotherapy techniques like dry needling, taping and support, strengthening the surrounding muscles with exercises that are appropriate for you, and supporting your understanding of how your back functions. Book a time to come see us to talk about your back pain and creating a treatment plan to reduce it. Have you or someone you love been diagnosed with multiple sclerosis? The symptoms of this condition can range from uncomfortable to debilitating. But the good news is that manual therapy techniques that fall under the scope of myotherapy can help to alleviate some of these symptoms. Let’s take a look at how myotherapy can help with multiple sclerosis. What is multiple sclerosis? Multiple sclerosis, or MS, is an autoimmune disorder that affects the central nervous system. ‘Sclerosis’ means ‘scars’, which occur throughout the central nervous system. These scars interfere with the nerve impulses within the brain, the spinal cord and the optic nerves. Because the scars can occur anywhere throughout the central nervous system, different symptoms can manifest. Over 25,000 Australians have been diagnosed with MS. Most are diagnosed between the ages of 20-40, but it can occur in people who are younger or older. Women are far more likely to be diagnosed with MS. What are the symptoms of multiple sclerosis? Because multiple sclerosis can occur throughout the nervous system, there is a wide range of symptoms that people with MS may experience. No two cases are the same. However, symptoms will typically fall under five main categories:
How can myotherapy help with multiple sclerosis? This can really depend on the primary symptoms you’re looking to manage. However, myotherapy has a diverse range of tools and techniques that may help to minimise symptoms related to motor control, fatigue and neurological issues. Some of the symptoms myotherapy may help to relieve include:
Massage and multiple sclerosis One of myotherapy’s tools that has some promising research to back it up is massage therapy. There have been several small studies into the benefits of massage therapy for MS. They found that massage therapy was able to relieve pain, fatigue and quality of life. One study found that massage was more effective at relieving symptoms compared to exercise therapy. It also suggested that combining massage with exercise therapy could have even greater benefits. Managing multiple sclerosis symptoms with Simple Wellness Myotherapy Here are Simple Wellness Myotherapy, we have had patient outcomes such as:
Every case of MS is unique, so we cannot guarantee that you will achieve the same results. But we can say that our practitioners are experienced when it comes to MS, and will go the extra mile to help you find as much relief as possible. Simple Wellness Myotherapy also works as a healthcare provider for those receiving employment assistance through MS Employment Services. If you are receiving employment assistance, you can have a chat with your Occupational Therapist to see if myotherapy can be incorporated into your package. Ready to make a booking? Click here to visit our booking page. You might be familiar with that sharp, shooting pain sensation in your lower back, hip and leg. It can also be felt as numbness, pins and needles, tingling or burning type of sensations. Whatever way the pain or symptoms present, it runs along the Sciatic nerve - which is why this is referred to as Sciatica.
But did you know theres more than one potential cause behind this pain? Often this pain can be linked to muscle tension in the glutes and hips. The Sciatic nerve runs underneath the muscles of your glutes, and when it gets compressed there it can be a real pain in the bum - literally! Because this nerve runs all the way down to your feet, the jolts of nerve pain can sometimes be felt anywhere from just localised in your buttocks and hip, to the back of your thigh, behind the knee, straight down your lower leg and even into the base of your foot. The Sciatic nerve can be impacted at the root of the nerve near the spine, however this doesn't always mean there will be pain. Often this is called a Bulging Disc or Herniated Disc, but you might be surprised to learn that even though "Bulging Disc" sounds pretty awful, studies have shown that more than 50% of people over 40 with no pain symptoms at all can have a disc bulge show on scans. Irritation or compression of the Sciatic nerve can be common after serious trauma to your leg or lower back. Things like car accidents, falls, and horse riding accidents are all common high impact incidents that can aggravate the nerve. If you've had an injury like this, its wise to seek treatment for it. Do you have Sciatic nerve pain or nerve symptoms of numbness, tingling and pins and needles? Book an appointment with us to have an assessment and treatment. If we can resolve the issue, we'll create you a treatment plan that includes manual therapies and a take home exercise program. More serious causes do exist, so if treatment of the muscles and joints is not relieving your pain, we'll refer you to see your GP to rule out any serious structural or pathological conditions. We all know that our bodies are full of these things called nerves, but have you ever wondered how they work to control your body?
Lets have a look at two important types of nerves in your body - the ones that tell you sensory information like touch or taste, and the ones that move your muscles and joints. Sensory nerves are responsible for everything you feel or sense. The five senses - sight, sound, touch, taste and smell - all fall under this category. Any awareness you have of the feeling or sensation of your body comes from the sensory nerves. The main sub types of these nerve receptors are mechanoreceptors, chemoreceptors and thermoreceptors. Mechanoreceptors respond to pressure and touch. When you feel muscles stretch out, or when you're aware of the chair you're sitting on, thats all thanks to mechanoreceptors. Chemoreceptors send information about chemical changes. This could be like the warming feeling of rubbing Deep Heat over your sore shoulder, as well as internal biochemical changes, like lactic acid build up after doing a big workout. Thermoreceptors tell us about temperature. They respond when you touch something hot or cold, and are the reason you'll quickly pull your hand away from a hot stove to avoid a serious burn. Then we have your Motor nerves, these are the ones that control movement. Every time you make a movement, its because these Motor nerves are sending a signal from your brain to the muscle they activate saying "Move!" Fun fact - muscles can only ever pull, they can't push! So when you activate your biceps to bend your elbow the biceps muscle contracts and gets shorter which pulls your forearm upwards. When you want to stretch your elbow back out straight, your Motor nerves activate your triceps which then pull your forearm back down to straighten the elbow. Everything in the body is controlled by nerve signals. The brain is like the control centre, and the nerves move out from the brain into all the tissue of your body - muscles, joints, organs, the lot. Some nerves can be over a metre long, like the ones that send signals to and from your toes. The nerves in your arms and hands all connect in via your neck, which is why we like to assess and treat your neck if you're having any pain, or tingling or other "nerve-y" symptoms in your hands and arms. The same goes from the nerves for your feet and legs - they extend out through your lower back, which is why we consider your back when you come in for treatment for your foot, ankle or leg. How can you tell if your pain or symptoms are nerve related? If a Sensory nerve is involved in your pain it can feel like sharp, shooting pains, tingling, pins and needles, numbness, or just feeling "weird" (we call that parasthesia) If its a Motor nerve thats involved, the muscle groups that nerve activates can be weak, or in extreme situations might not be able to activate at all. If you think your symptoms may be nerve related, book in with your Myotherapist for a full assessment and treatment plan. Everyone has experienced pain at one time or another. But pain is personal – each of us experiences pain differently. Some of us feel it very intensely, and others not so much. This is because pain depends not only on what happens to your body, but also how your brain responds to it. This is what is known as the Pain Matrix. What is the Pain Matrix?
This matrix processes information from the nerves that tell us when we’re in danger or injured. It responds by increasing or decreasing our sensitivity to these messages. These changes – known as top-down regulation – control how intensely we feel pain. The Pain Matrix involves different areas of the brain that control emotions, behaviour, movement, perception and thoughts. So it’s no surprise that when you’re in pain, all of these different factors can change. How does the Pain Matrix work? There are two main changes that the Pain Matrix can induce. Anti-nociception is a reduction in sensitivity to pain, whereas pro-nociception is an increase. Anti-nociception uses the body’s natural painkillers – endorphins – to block the danger signal and decrease the pain response. Ever seen someone injure themselves in a dangerous situation, like in a car accident, but they can still move to safety without feeling pain? This is because a rush of endorphins temporarily blocks out the message of danger so they can get to safety. On the other hand, pro-nociception is usually due to swelling and chemical changes in the nerve endings around an injury. Have you ever had a bad paper-cut? Your sensitivity is much higher around the cut, even if you’re not touching the injured part. Sometimes, even moving the other fingers can hurt. Changes in the brain = changes in the pain Despite what we used to believe, the brain can continually change its form and function as a form of adaptation. These changes are known as Neuroplasticity. Nerve pathways can physical alter by increasing or reducing the number of connections. Or they can alter the release of neurotransmitters – more stimulating neurotransmitters means more nerve activity, which can increase the sensitivity of the system. When it comes to chronic pain conditions, the central nervous system is reorganised. This can include damage to nerves, leading to abnormal connections between them. Pain is more likely to occur than not, as pro-nociception increases and anti-nociception is impaired. This can lead to exaggerated responses to pain including pain caused by non-painful experiences - this is known as allodynia, and can be a common symptom in conditions like Fibromyalgia. Long term inflammation can lead to a heightened sensitivity of the nervous system. In the presence of inflammation the amount of nerve stimulation needed to send the signal decreases and the nerve firing rate increases. With so many danger messages coming in when there is inflammation present, the nervous system starts to respond on high alert by using its protective mechanism - pain! Controlling the pain There is no one size fits all approach to controlling pain, but theres increasing evidence that changes to pain intensity can be influenced by more than just the incoming messages from our tissue - it can also be influenced by our perceptions of danger and safety. This is likely due to the pain matrixes involvement in areas of the brain that deal with emotions, behaviours and thoughts. Pain experts Dr Lorimer Moseley and Dr David Butler of the NOI Group have published a fantastic book called Explain Pain that describes DIMs and SIMs - that is, Danger In Me (DIMs) and Safety In Me (SIMs). They say that any credible indication of danger can increase your perception of pain, and likewise a credible indication of safety can decrease the pain. We'll dive deeper into this research in future blogs. The Gate Control Theory involves a more physical approach to pain control. Have you ever bumped into something, then rubbed the area to make it hurt less? The Gate Control Theory is that non-painful sensations such as pressure can block or override the danger messages and reduce pain. The nerves that tell us about pressure are faster and more effective than those that tell us about danger. This might be part of why something like a good massage session helps with pain. Massage is also a great way to stimulate some feel-good endorphins, which promotes anti-nociception to reduce painful sensations! If you’re looking to minimise your pain, a combination of massage, exercise therapy and other myotherapy treatments can help. Have a look at my online booking calendar to book in for an appointment. The human body is a confusing thing! Some things that don’t seem that concerning to you might be a warning sign for your practitioner. It can be difficult to tell what just needs a heat pack or a cup of tea, what needs a practitioner and what needs an emergency room visit! What is meant by the term "red flag"? Its a sign or symptom that can indicate the possibility of a serious medical condition that may be dangerous if left unchecked. So today I will discuss some of the most common red flag signs and symptoms I see as a myotherapist. If you are experiencing these types of symptoms, its always safest to check in with your GP first. Severe Pain
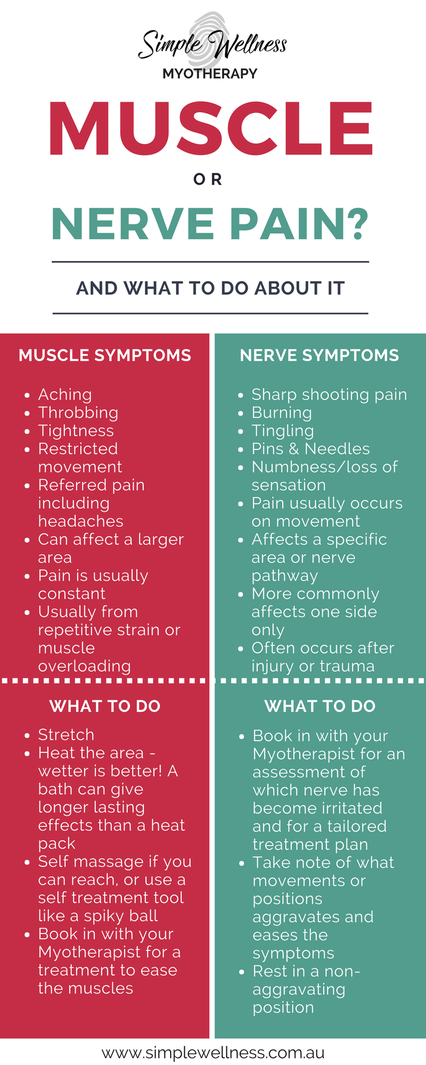
This might seem a little obvious. But sudden, severe pain is always a red flag, even if you think you know the cause. If it causes nausea, vomiting or loss of consciousness, you need to seek medical attention, stat. Night Time Pain That Wakes You Up Pain that wakes you up, stops you from falling asleep, or doesn't ease with rest is an indicator that something is not right. It can be associated with infection, inflammation, abdominal aortic aneurysm and cancer. Sudden Changes In Bladder/Bowel Control In myotherapy terms, this is a very serious red flag. Although there can be more benign reasons for a change in bladder or bowel control, it could be a sign of serious nerve or spinal damage. Seek out your GP asap. Dizziness & Fainting Spells There can be may reasons why you experience dizziness and fainting. Some can be as simple as low blood pressure. But some can be a warning sign of something nastier. If you lose consciousness completely, then you need to seek immediate medical attention. For dizzy spells, book in to see your GP for a general checkup. Burning Soles Of Feet It seems like the least significant of the listed red flags. But this one can be just as serious. Burning soles can be a sign of nerve dysfunction in the legs, spine or feet. But it can also be a warning sign for deep vein thrombosis – a blood clot that occurs in a vein. If DVT is not treated, it can be fatal. So don’t hesitate to get a medical check-up straight away. Lower-Mid Back Pain Plus Altered Urination This might seem like an unusual combination of symptoms. But it can involve serious kidney involvement – from a kidney infection to kidney disease and even kidney failure. If your lower-mid back pain is still lingering after a treatment, its worth considering that it may be kidney related. If in doubt, get some tests done to check your kidney function, its always better to check it out than leave it to progress! Chest Pain & Shortness Of Breath It’s not just the dramatic heart-clutching Hollywood-style chest pain that is a red flag. Any unexpected chest pain is a concern, whether it feels obviously muscular or deeper into the chest. Difficulty breathing can also be a major concern – after all, we need enough oxygen to function! For mild cases, you can seek your GP’s attention immediately. But if in doubt, call 000 – better to be safe than sorry. Severe Headaches We all get headaches from time to time. But severe headaches can be a sign of issues including hormone imbalances, nerve dysfunction or even brain tumours. The more severe the headache, the sooner you should seek medical attention. Even if you are used to having migraines, it is still a red flag to get suddenly what feels like the worst headache you will ever experience. Feeling confused, running a fever, vomiting and numbness associated with a headache means you need to seek help immediately. Sudden Changes In Vision Seeing is a pretty important part of surviving in today’s world. But if there are sudden changes to your vision such as blurriness, double vision or loss of vision (even temporarily), it can mean that something is impairing the function of your eyes or your brain. Look out for co-existing symptoms along with vision changes - like headache, dizziness, or nausea. If you are experiencing any changes in vision, please do not drive anywhere, even to seek medical help. Order an Uber or a cab, ask a friend for a lift, or if all else fails, call an ambulance or book a home visit with a GP. Significant Weakness/Numbness Muscle weakness when you have worked out or numbness when you’ve been sitting on your foot is one thing. But if you experience unexpected weakness, numbness or inability to move any body part, it’s a massive red flag. This shows that your nerves are not functioning properly or your nervous system isn’t getting the message. If any area of your body feels numb, this is a sign of nerve involvement. Numb can mean different things to different people, but usually people describe it to me as being like pins and needles, a bit tingly, feeling "different" or a true numbness of complete loss of feeling. The most common areas to have this numbness is in the arms and legs, and usually it starts at the fingers and toes. This is a kind of red flag that your myotherapist may be able to help you out with, although you may still need to see your GP or your Chiropractor if any scans are required or if structural treatment is needed. If you experience any of these symptoms, your first stop should be your GP. If you come in to see me and we can't clear these red flag symptoms, I might not be able to treat you. But once you’ve got the all-clear, I’m happy to help with any musculoskeletal symptoms. To book in a session, head here. Pain is sucky – no matter what it is. But sometimes it’s good to know your pain, so you know how urgently you need to act on it. One of the most common questions about pain is how can you tell if it’s muscle pain or nerve pain? The best option is always to ask someone who can check for you – like me! But there are some ways you might be able to tell the difference. Muscle Pain It’s pretty common to experience muscle pain. It might be as subtle as an ache after a workout, or it could be agony if you’ve torn a muscle. The way to recognise muscle pain is that it is generally:
Nerve Pain Nerve pain is usually of greater concern, as your nerves hurting is a sign that something is compressing or impinging a nerve somewhere in the body. If you’re experiencing nerve pain, it is generally:
The two types of pain can exist separately, or you might experience a mix of both. But both are a sign that the body is not happy with something. I’m In Pain Right Now. What Can I Do To Relieve It? Pain is a signal that lets you know something might not be right and needs protection. If it’s a mild pain, there’s no need to panic. But if it’s unexpected pain, nerve pain or related to a chronic condition, your first step is to book in with your practitioner. Getting treatment right away helps to reduce your pain quicker. Your practitioner can advise you on some safe at home care practices, but if you can't get a booking at short notice there are still steps you can take. Whether its muscle or nerve pain, the basic DIY first aid for your pain is the same. So until you are able to get it looked after, you should:
These will help to ease the pain and prevent further damage until you’re able to get in and get it checked out properly. You’ll see that I didn’t include ice in there. There is emerging research that shows that ice may not always be the best option for treating injuries and pain. So if you want to add on some temperature relief, it’s up to you – you might feel like ice gives you some relief, or you might prefer a heat pack, or you may find best relief using an alternating combination of the two. Once I’ve assessed your pain, I will let you know which might be better for you. The guide below is a quick way of doing the investigative work on whether your pain is muscle or nerve related, but its always best to consult with a health professional rather than trusting good old Doctor Google. You don’t have to just grit your teeth through any sort of pain. As a qualified myotherapist, I can help to relieve your symptoms and get you back on track to health. So book in an appointment today – you won’t regret it!
|
Meet Our Team
We have a team of great practitioners available 7 days a week at our Rowville clinic. Archives
July 2024
Categories
All
|
Got a question about Myotherapy?
Contact Mel by phone, email or Facebook
|
Simple Wellness Myotherapy & Remedial Massage Clinic
Shop 12B 150 Kelletts Rd Rowville VIC 3178 |
Phone us on
03 8204 0970 |


 RSS Feed
RSS Feed